Global Revenue Cycle Management Market, By Offering, By Deployment Model, By Application, By End User, By Region & Segmental Insights Trends and Forecast, 2024 – 2034
- Industry: Healthcare
- Report ID: TNR-110-1173
- Number of Pages: 420
- Table/Charts : Yes
- June, 2024
- Base Year : 2024
- No. of Companies : 10+
- No. of Countries : 29
- Views : 10116
- Covid Impact Covered: Yes
- War Impact Covered: Yes
- Formats : PDF, Excel, PPT
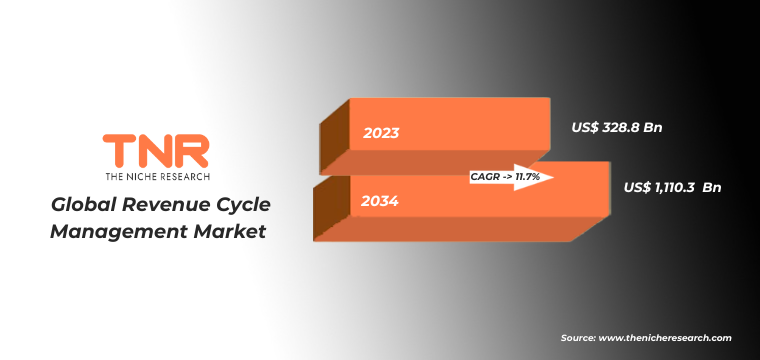
In Terms of Revenue, the Global Revenue Cycle Management Market was Worth US$ 328.8 Bn in 2023 and is Anticipated to Witness a CAGR of 11.7% During 2024 – 2034.
The revenue cycle management (RCM) market encompasses the technology and services used by healthcare providers to manage financial processes such as patient registration, insurance verification, claims processing, and payment collection. It plays a crucial role in ensuring the financial health of healthcare organizations by optimizing revenue generation and streamlining administrative workflows. The RCM market has been experiencing robust growth due to several factors. Firstly, the increasing adoption of electronic health records (EHR) and healthcare IT solutions has driven the demand for integrated RCM systems. These systems help in automating and improving billing accuracy, reducing claim denials, and accelerating reimbursement cycles.
Regulatory requirements and the shift towards value-based care models have spurred healthcare providers to invest in RCM solutions that enhance operational efficiency and compliance. A notable trend in the RCM market is the integration of artificial intelligence (AI) and machine learning (ML) capabilities to automate mundane tasks, predict payment behaviors, and optimize revenue workflows further. Cloud-based RCM solutions are gaining popularity due to their scalability, cost-effectiveness, and ease of implementation across different healthcare settings. Overall, the RCM market is poised for continued growth as healthcare organizations seek to enhance financial performance amidst evolving regulatory landscapes and patient care demands.
Revenue Cycle Management Market Dynamic
Growth Driver-
Increasing Complexity and Volume of Healthcare Data
As healthcare providers transition towards digital systems like electronic health records (EHRs) and practice management software, they generate vast amounts of patient information and financial data. Managing this data manually is challenging and prone to errors, leading to delays in claims processing, higher denial rates, and increased administrative costs.
RCM solutions equipped with advanced analytics and automation capabilities help healthcare organizations navigate this complexity more efficiently. They enable real-time data analysis to identify trends, predict payment behaviors, and optimize revenue cycles. By leveraging technology to streamline billing processes, reduce claim denials, and improve overall financial performance, RCM solutions are becoming indispensable for healthcare providers seeking to enhance operational efficiency and maintain financial stability in an increasingly data-driven healthcare landscape. Thus, the growing demand for effective data management solutions continues to propel the expansion of the RCM market.
Trends-
Increasing Complexity and Volume of Healthcare Data
As healthcare providers transition towards digital systems like electronic health records (EHRs) and practice management software, they generate vast amounts of patient information and financial data. Managing this data manually is challenging and prone to errors, leading to delays in claims processing, higher denial rates, and increased administrative costs.
RCM solutions equipped with advanced analytics and automation capabilities help healthcare organizations navigate this complexity more efficiently. They enable real-time data analysis to identify trends, predict payment behaviors, and optimize revenue cycles. By leveraging technology to streamline billing processes, reduce claim denials, and improve overall financial performance, RCM solutions are becoming indispensable for healthcare providers seeking to enhance operational efficiency and maintain financial stability in an increasingly data-driven healthcare landscape. Thus, the growing demand for effective data management solutions continues to propel the expansion of the RCM market.
Challenge-
Increasing Emphasis on Patient-Centric Approaches and Consumerism
Healthcare consumers are demanding more transparency and convenience in billing and payment processes, similar to other consumer-oriented industries. This trend is pushing healthcare providers to adopt RCM solutions that prioritize patient engagement, satisfaction, and financial transparency.
RCM systems are evolving to offer patients easier access to their billing information, clear explanations of costs, and multiple payment options. Providers are integrating patient portals and mobile applications into their RCM strategies to enhance communication and empower patients to manage their healthcare finances more effectively. Moreover, personalized billing and payment plans are being implemented to accommodate diverse patient needs and financial situations, fostering stronger patient-provider relationships and improving overall patient satisfaction. As patient expectations continue to shape healthcare delivery, RCM solutions that prioritize consumer-centric features are gaining traction and driving market growth.
Revenue Cycle Management Market Segmentation by Offering, Deployment Model, Application, End User, Region
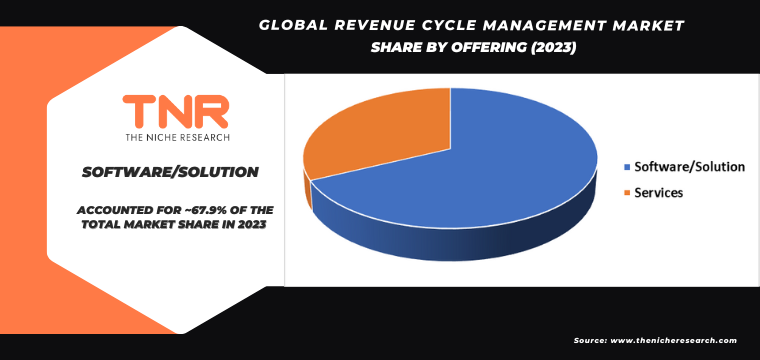
Software/solution segment by offering is set to dominate the revenue cycle management market, commanding a substantial revenue share of 67.9% over the forecast period.
Healthcare organizations are increasingly investing in RCM software to streamline administrative workflows, improve billing accuracy, reduce claim denials, and accelerate reimbursement cycles. Integrated RCM software also supports compliance with evolving healthcare regulations and facilitates seamless interoperability with electronic health records (EHR) and other healthcare IT systems. Moreover, advancements in technology such as artificial intelligence (AI) and machine learning (ML) are enhancing the functionality of RCM software, enabling predictive analytics and automation that further optimize revenue cycle operations. As healthcare providers prioritize efficiency and financial performance, the software/solution segment of the RCM market is poised to maintain its dominance and continue expanding over the forecast period.
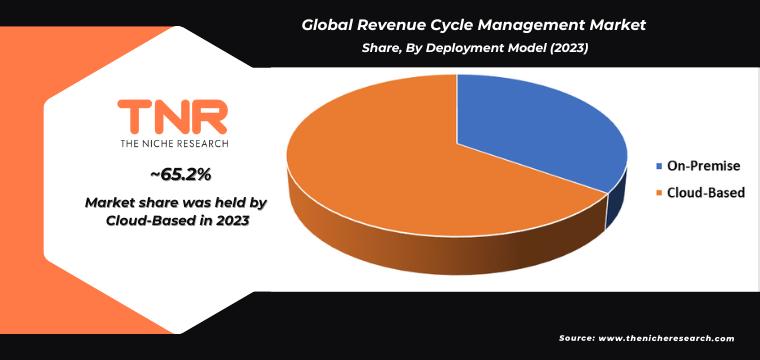
Cloud-based segment by deployment model is set to dominate the revenue cycle management market, commanding a substantial revenue share of 65.2% over the forecast period.
Cloud-based RCM solutions offer significant advantages, including scalability, flexibility, and cost-effectiveness. Healthcare providers can scale their RCM infrastructure as needed without large upfront investments in hardware or IT resources, making cloud solutions particularly attractive. Cloud-based RCM systems facilitate easier integration with existing healthcare IT systems, such as electronic health records (EHRs), practice management systems, and patient portals.
This integration improves data accessibility and interoperability, streamlines workflows, and enhances overall operational efficiency. Cloud deployments also ensure data security and compliance with healthcare regulations through robust encryption protocols and regular updates by cloud service providers. As healthcare organizations increasingly prioritize agility, cost savings, and data security, the cloud-based deployment model is expected to dominate the RCM market, maintaining its growth trajectory over the forecast period.
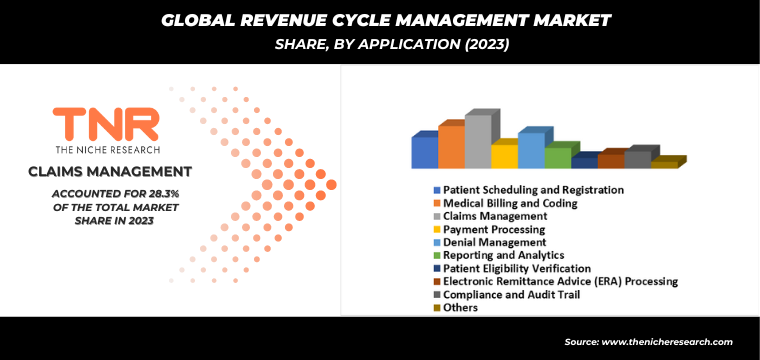
Medical billing and coding by application category is anticipated to be the fastest-growing segment in the revenue cycle management market, capturing a substantial revenue share of 16.6% over the forecast period.
There’s a growing emphasis on accuracy and efficiency in healthcare billing processes to minimize claim denials and optimize revenue cycles. Medical billing and coding systems automate the complex process of translating healthcare services into standardized codes for billing purposes, reducing errors and improving reimbursement rates. Regulatory changes and compliance requirements in healthcare necessitate robust billing and coding solutions that ensure adherence to evolving standards. Healthcare providers are increasingly investing in advanced RCM technologies that integrate medical billing and coding functionalities with other RCM components like patient registration and claims management.
This integration enhances workflow efficiency, accelerates reimbursement timelines, and supports overall financial health for healthcare organizations. As healthcare delivery becomes more data-driven and regulations continue to evolve, the demand for efficient medical billing and coding solutions is expected to drive substantial growth in this segment of the RCM market over the forecast period.
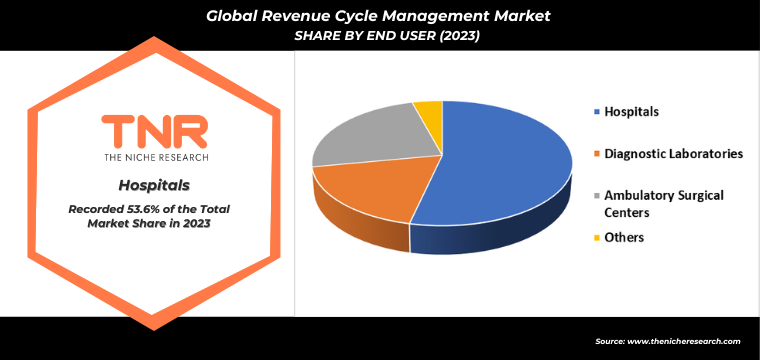
Hospitals segment dominated the revenue cycle management market, capturing a significant revenue share of 53.6% over the forecast period.
Hospitals typically handle a large volume and variety of patient cases, procedures, and billing complexities compared to other healthcare settings. This complexity necessitates robust RCM solutions to streamline revenue processes, enhance billing accuracy, and reduce administrative costs. Moreover, hospitals often have diverse revenue streams from various services, including inpatient, outpatient, emergency care, and specialized treatments.
Effective RCM solutions tailored for hospitals integrate seamlessly with electronic health records (EHRs), clinical systems, and billing platforms, optimizing revenue capture and cycle management across different departments and specialties. As hospitals continue to focus on improving operational efficiency, financial performance, and patient care outcomes, the demand for comprehensive RCM solutions tailored to hospital settings is expected to maintain its dominance in the market over the forecast period.
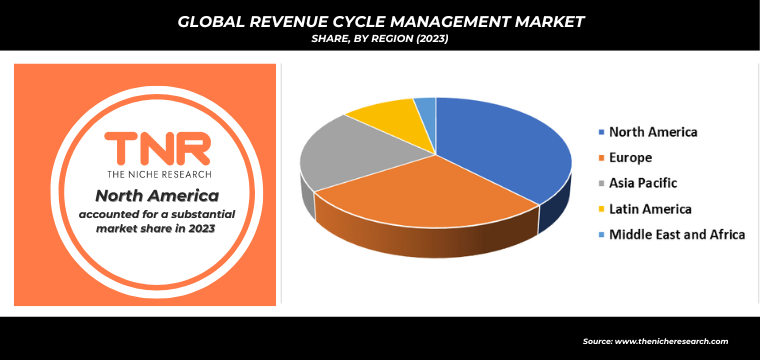
In 2023, North America is anticipated to play a significant role in propelling the growth of the revenue cycle management market, contributing approximately 37.7% to its overall expansion.
North America boasts a mature healthcare infrastructure that embraces advanced technologies, including electronic health records (EHR) and integrated RCM systems. Secondly, stringent regulatory requirements in the healthcare sector drive the adoption of RCM solutions to ensure compliance and streamline financial operations. The presence of leading RCM solution providers and a robust ecosystem of healthcare organizations eager to optimize revenue cycles further fuels market growth. Investments in healthcare IT and digital transformation initiatives also play a crucial role in enhancing operational efficiency and patient care outcomes. Overall, North America’s proactive approach to healthcare technology adoption and regulatory adherence positions it as a cornerstone of innovation and growth within the global RCM market landscape.
Key Developments
- In June 2022, R1 RCM Inc completed the acquisition of Cloudmed, aiming to enhance its capabilities in healthcare provider revenue cycle management (RCM) and accelerate digital transformation through automation and AI technologies.
- In July 2020, GeBBS Healthcare Solutions, Inc., entered into a partnership with INTEGRIS Health for revenue cycle management (RCM). GeBBS will deliver strategic outsourcing solutions aimed at optimizing INTEGRIS Health’s revenue cycle. By utilizing technology-enabled innovative approaches, the partnership seeks to decrease operational and capital expenditures, recover lost revenue, enhance patient satisfaction, and boost overall productivity.
Major Players in Revenue Cycle Management Market
- athenahealth, Inc.
- CareCloud, Inc.
- Epic Systems Corporation
- Experian Information Solutions, Inc.
- McKesson Corporation
- NXGN Management, LLC
- Oracle (Cerner Corporation)
- Passage Health International, L.L.C.
- Quest Diagnostics, Inc.
- R1 RCM Inc.
- The SSI Group, Inc.
- Veradigm LLC (AllScripts Healthcare, LLC)
- Other Industry Participants
Global Revenue Cycle Management Market Scope
| Report Specifications | Details |
| Market Revenue in 2023 | US$ 328.8 Bn |
| Market Size Forecast by 2034 | US$ 1,110.3 Bn |
| Growth Rate (CAGR) | 11.7% |
| Historic Data | 2016 – 2022 |
| Base Year for Estimation | 2023 |
| Forecast Period | 2024 – 2034 |
| Report Inclusions | Market Size & Estimates, Market Dynamics, Competitive Scenario, Trends, Growth Factors, Market Determinants, Key Investment Segmentation, Product/Service/Solutions Benchmarking |
| Segments Covered | By Offering, By Deployment Model, By Application, By End User, By Region |
| Regions Covered | North America, Europe, Asia Pacific, Middle East & Africa, Latin America |
| Countries Covered | U.S., Canada, Mexico, Rest of North America, France, The UK, Spain, Germany, Italy, Nordic Countries (Denmark, Finland, Iceland, Sweden, Norway), Benelux Union (Belgium, The Netherlands, Luxembourg), Rest of Europe, China, Japan, India, New Zealand, Australia, South Korea, Southeast Asia (Indonesia, Thailand, Malaysia, Singapore, Rest of Southeast Asia), Rest of Asia Pacific, Saudi Arabia, UAE, Egypt, Kuwait, South Africa, Rest of Middle East & Africa, Brazil, Argentina, Rest of Latin America |
| Key Players | athenahealth, Inc. CareCloud, Inc., Epic Systems Corporation, Experian Information Solutions, Inc., McKesson Corporation, NXGN Management, LLC, Oracle (Cerner Corporation), Passage Health International, L.L.C., Quest Diagnostics, Inc., R1 RCM Inc., The SSI Group, Inc., Veradigm LLC (AllScripts Healthcare, LLC) |
| Customization Scope | Customization allows for the inclusion/modification of content pertaining to geographical regions, countries, and specific market segments. |
| Pricing & Procurement Options | Explore purchase options tailored to your specific research requirements |
| Contact Details | Consult With Our Expert
Japan (Toll-Free): +81 663-386-8111 South Korea (Toll-Free): +82-808- 703-126 Saudi Arabia (Toll-Free): +966 800-850-1643 United Kingdom: +44 753-710-5080 United States: +1 302-232-5106 E-mail: askanexpert@thenicheresearch.com
|
Global Revenue Cycle Management Market
By Offering
- Software/Solution
- Integrated
- Standalone
- Services
- Consulting
- Implementation
- Support and Maintenance
- Others
By Deployment Model
- On-Premise
- Cloud-Based
By Application
- Patient Scheduling and Registration
- Medical Billing and Coding
- Claims Management
- Payment Processing
- Denial Management
- Reporting and Analytics
- Patient Eligibility Verification
- Electronic Remittance Advice (ERA) Processing
- Compliance and Audit Trail
- Others
By End User
- Hospitals
- Diagnostic Laboratories
- Ambulatory Surgical Centers
- Others
By Region
- North America (U.S., Canada, Mexico, Rest of North America)
- Europe (France, The UK, Spain, Germany, Italy, Nordic Countries (Denmark, Finland, Iceland, Sweden, Norway), Benelux Union (Belgium, The Netherlands, Luxembourg), Rest of Europe)
- Asia Pacific (China, Japan, India, New Zealand, Australia, South Korea, Southeast Asia (Indonesia, Thailand, Malaysia, Singapore, Rest of Southeast Asia), Rest of Asia Pacific)
- Middle East & Africa (Saudi Arabia, UAE, Egypt, Kuwait, South Africa, Rest of Middle East & Africa)
- Latin America (Brazil, Argentina, Rest of Latin America)
Report Layout:
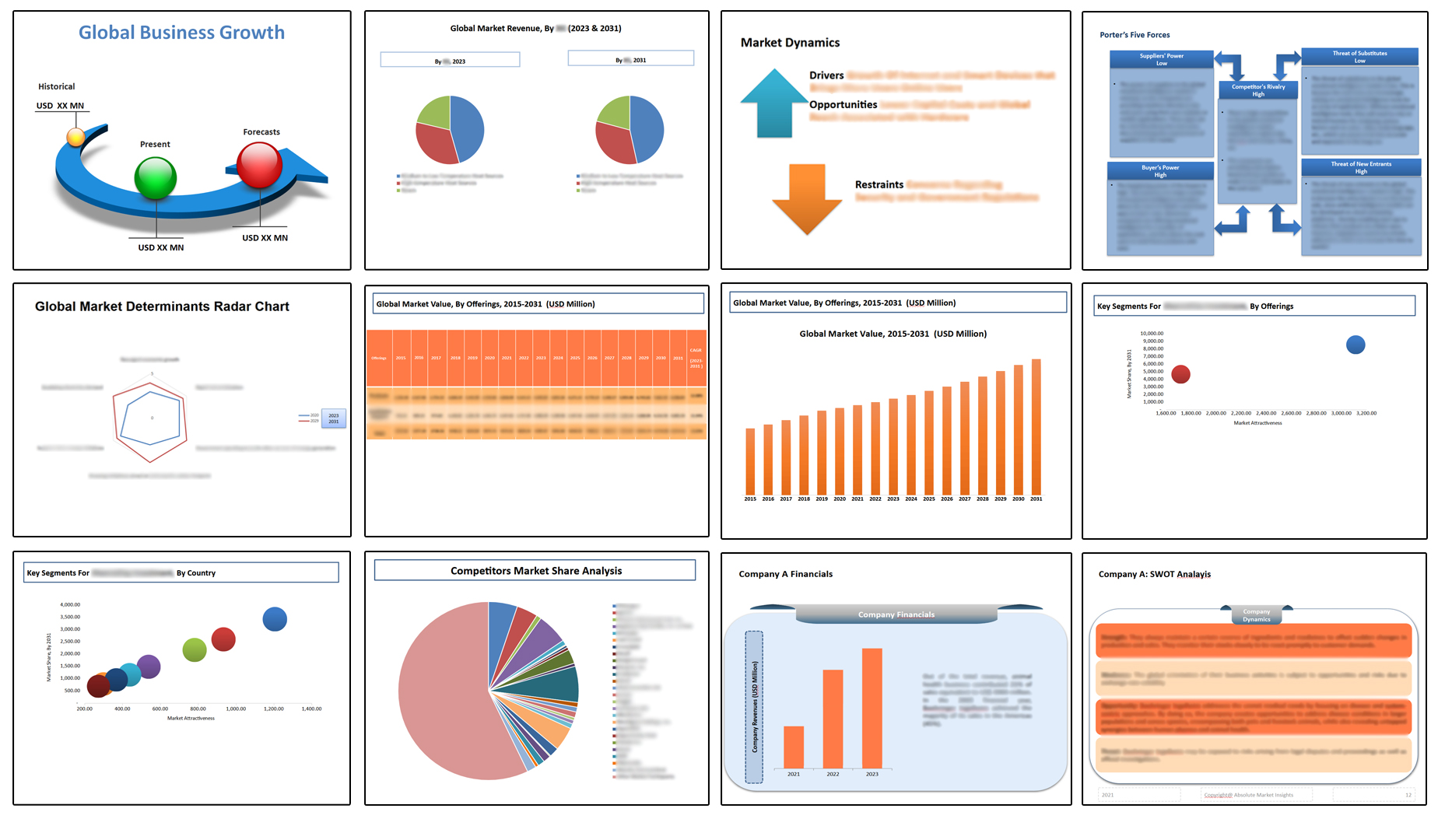
Table of Contents
Note: This ToC is tentative and can be changed according to the research study conducted during the course of report completion.
**Exclusive for Multi-User and Enterprise User.
Global Revenue Cycle Management Market
By Offering
- Software/Solution
- Integrated
- Standalone
- Services
- Consulting
- Implementation
- Support and Maintenance
- Others
By Deployment Model
- On-Premise
- Cloud-Based
By Application
- Patient Scheduling and Registration
- Medical Billing and Coding
- Claims Management
- Payment Processing
- Denial Management
- Reporting and Analytics
- Patient Eligibility Verification
- Electronic Remittance Advice (ERA) Processing
- Compliance and Audit Trail
- Others
By End User
- Hospitals
- Diagnostic Laboratories
- Ambulatory Surgical Centers
- Others
By Region
- North America (U.S., Canada, Mexico, Rest of North America)
- Europe (France, The UK, Spain, Germany, Italy, Nordic Countries (Denmark, Finland, Iceland, Sweden, Norway), Benelux Union (Belgium, The Netherlands, Luxembourg), Rest of Europe)
- Asia Pacific (China, Japan, India, New Zealand, Australia, South Korea, Southeast Asia (Indonesia, Thailand, Malaysia, Singapore, Rest of Southeast Asia), Rest of Asia Pacific)
- Middle East & Africa (Saudi Arabia, UAE, Egypt, Kuwait, South Africa, Rest of Middle East & Africa)
- Latin America (Brazil, Argentina, Rest of Latin America)
The Niche Research approach encompasses both primary and secondary research methods to provide comprehensive insights. While primary research is the cornerstone of our studies, we also incorporate secondary research sources such as company annual reports, premium industry databases, press releases, industry journals, and white papers.
Within our primary research, we actively engage with various industry stakeholders, conducting paid interviews and surveys. Our meticulous analysis extends to every market participant in major countries, allowing us to thoroughly examine their portfolios, calculate market shares, and segment revenues.
Our data collection primarily focuses on individual countries within our research scope, enabling us to estimate regional market sizes. Typically, we employ a bottom-up approach, meticulously tracking trends in different countries. We analyze growth drivers, constraints, technological innovations, and opportunities for each country, ultimately arriving at regional figures.Our process begins by examining the growth prospects of each country. Building upon these insights, we project growth and trends for the entire region. Finally, we utilize our proprietary model to refine estimations and forecasts.
Our data validation standards are integral to ensuring the reliability and accuracy of our research findings. Here’s a breakdown of our data validation processes and the stakeholders we engage with during our primary research:
- Supply Side Analysis: We initiate a supply side analysis by directly contacting market participants, through telephonic interviews and questionnaires containing both open-ended and close-ended questions. We gather information on their portfolios, segment revenues, developments, and growth strategies.
- Demand Side Analysis: To gain insights into adoption trends and consumer preferences, we reach out to target customers and users (non-vendors). This information forms a vital part of the qualitative analysis section of our reports, covering market dynamics, adoption trends, consumer behavior, spending patterns, and other related aspects.
- Consultant Insights: We tap into the expertise of our partner consultants from around the world to obtain their unique viewpoints and perspectives. Their insights contribute to a well-rounded understanding of the markets under investigation.
- In-House Validation: To ensure data accuracy and reliability, we conduct cross-validation of data points and information through our in-house team of consultants and utilize advanced data modeling tools for thorough verification.
The forecasts we provide are based on a comprehensive assessment of various factors, including:
- Market Trends and Past Performance (Last Five Years): We accurately analyze market trends and performance data from preceding five years to identify historical patterns and understand the market’s evolution.
- Historical Performance and Growth of Market Participants: We assess the historical performance and growth trajectories of key market participants. This analysis provides insights into the competitive landscape and individual company strategies.
- Market Determinants Impact Analysis (Next Eight Years): We conduct a rigorous analysis of the factors that are projected to influence the market over the next eight years. This includes assessing both internal and external determinants that can shape market dynamics.
- Drivers and Challenges for the Forecast Period:Identify the factors expected to drive market growth during the forecast period, as well as the challenges that the industry may face. This analysis aids in deriving an accurate growth rate projection.
- New Acquisitions, Collaborations, or Partnerships: We keep a close watch on any new acquisitions, collaborations, or partnerships within the industry. These developments can have a significant impact on market dynamics and competitiveness.
- Macro and Micro Factors Analysis:A thorough examination of both macro-level factors (e.g., economic trends, regulatory changes) and micro-level factors (e.g., technological advancements, consumer preferences) that may influence the market during the forecast period.
- End-User Sentiment Analysis: To understand the market from the end-user perspective, we conduct sentiment analysis. This involves assessing the sentiment, preferences, and feedback of the end-users, which can provide valuable insights into market trends.
- Perspective of Primary Participants: Insights gathered directly from primary research participants play a crucial role in shaping our forecasts. Their perspectives and experiences provide valuable qualitative data.
- Year-on-Year Growth Trend: We utilize a year-on-year growth trend based on historical market growth and expected future trends. This helps in formulating our growth projections, aligning them with the market’s historical performance.
Research process adopted by TNR involves multiple stages, including data collection, validation, quality checks, and presentation. It’s crucial that the data and information we provide add value to your existing market understanding and expertise. We have also established partnerships with business consulting, research, and survey organizations across regions and globally to collaborate on regional analysis and data validation, ensuring the highest level of accuracy and reliability in our reports.